What is Thyroid Eye Disease? (Also known as Graves’ Ophthalmopathy or Graves’ Eye Disease)
Thyroid eye disease (TED), also known as Graves’ ophthalmopathy or Graves’ Eye Disease, is an autoimmune disease in which the immune system causes inflammation and swelling which leads to abnormalities within muscle tissue and fat behind the eye. An overactive thyroid gland (hyperthyroidism) is usually caused by Graves’ disease. Up to one-half of people with Graves’ disease develop thyroid eye disease (TED). In some people, thyroid eye disease can occur with normal levels of thyroid hormones (euthyroid) or low levels of thyroid hormones (hypothyroidism). Thyroid eye disease may occur in patients who already know they have thyroid disease, or it may be the first sign of Graves’ disease. While TED often occurs in people living with hyperthyroidism or Graves’ disease, it is a distinct disease and treating hyperthyroidism may not resolve the TED symptoms and signs.
[aiovg_video id=56395]
Parts of the Eye
Fact Sheets to Share and Print
The main symptoms of thyroid eye disease include inflammation an an increase in the muscle and fat behind the eye (in the bony eye socket), often causing the eyeballs to push forward. If the eye is pushed far enough forward, the eyelids may not close properly when blinking and sleeping. The clear front part of the eye, called the cornea, may become unprotected, dry, and damaged. Stiffening and inflammation of the muscles of the eye may prevent them from working well, affecting eye position and eye movements and leading to double vision. In severe cases, the inflammation and increase in the tissues, muscles, and fat behind the eye compresses the optic nerve, the nerve that connects the eye to the brain, causing vision loss.
Who is at Risk for Thyroid Eye Disease (TED)?
Thyroid eye disease is most commonly associated with Graves’ disease. However, it can also occur without a diagnosis of Graves’ disease
Other risk factors for thyroid eye disease (TED) include:
- Age: Usually affects middle-aged adults but can occur at any age
- Gender: Females are affected more than males
- Family history of thyroid eye disease
- Smoking: Smoking increases the risk of thyroid eye disease by 7–8 times, causes thyroid eye disease to have a longer “active phase”, and it reduces the effectiveness of treatments
- Radioactive iodine therapy: Radioactive iodine has been used to treat hyperthyroidism and Graves’ disease. This treatment should be used with caution in people with TED as it may worsen the condition unless steroids are given at the same time
- Low blood levels of selenium, a dietary mineral
- Low blood levels of vitamin D
[aiovg_video id=”56132″]
What are the Symptoms of Thyroid Eye Disease (TED)?
Symptoms of thyroid eye disease (TED) are caused by the tissues, fat, and muscles of the eye socket swelling and pushing the eyeball forward. Tissues around the eye also may swell and become thickened. It is not unusual for symptoms to be worse in one eye than the other. TED changes over time, with symptoms that can appear anytime and range from mild to severe. The appearance of thyroid eye disease can be different for each person. TED symptoms may include:
Dry, gritty and irritated eyes
Red eyes
Watery eyes
Puffy eyelids
Sensitivity to light
Bulging eyes (called proptosis) and lid retraction – giving a staring or startled appearance
Double vision
In more severe thyroid eye disease, there may also be:
- Trouble moving eyes and closing eyes
- Inability to completely close your eye causing corneal exposure or even an ulcer
- Blurred or loss of vision due to optic nerve compression (colors may appear dull or dim), or corneal damage from an ulcer, leading to scarring
If you have Graves’ disease, eye symptoms most often begin within six months of disease diagnosis. Very rarely, eye problems may develop long after the Graves’ disease has been treated. In some patients with eye symptoms, hyperthyroidism never develops and, rarely, patients may have hypothyroidism. The severity of the eye symptoms is not related to the severity of the hyperthyroidism.
How is Thyroid Eye Disease (TED) Diagnosed?
If you have thyroid disease or suspect that you may have TED, your doctor may recommend that you see an eye doctor (ophthalmologist). Thyroid eye disease is managed by an ophthalmologist. Management of more severe forms of the disease may require a team of ophthalmologists, including specialists in eye plastic surgery, eye muscle surgery, and neuro-ophthalmology. They will be able to evaluate your symptoms, recommend a course of treatment, discuss surgical options to improve eye function and appearance, and help you watch for any problems with decreased vision.
How is Thyroid Eye Disease (TED) Treated and Managed?
In its severe form, thyroid eye disease can last between one and three years. That means if it is left untreated, the inflammation may gradually decrease by itself but may cause damage to vision through the course of the disease. Inflammation also can flare up later. Sometimes, the changes caused by the enlargement of the tissues (such as bulging eyes or double vision) may not go away. The goal of treatment is to limit severe inflammation and swelling and to protect the front of the eye and prevent vision loss.
Thyroid eye disease is managed by an ophthalmologist. Any underlying thyroid problems will be managed by your primary care doctor (PCP) or by a specialist in the hormone systems of the body (an endocrinologist).
If a thyroid issue is suspected, evaluation and treatment are critical. The first priority is to restore your normal thyroid function. In addition, eye conditions should be examined and treated at the same time as your thyroid gland treatment. Eye problems may continue to progress even after your thyroid function returns to normal.
If you have TED, your ophthalmologist may recommend one or more of the following treatments to help soothe your eyes and improve your vision:
Cool compresses: Apply cool compresses to your eyes. The extra moisture and cooling effect may provide relief.
Sunglasses: When you have thyroid eye disease, your eyes are more sensitive to sunlight and UV rays. Wearing sunglasses helps protect your eyes from both sun and wind.
Lubricating eye drops: Use lubricating eye drops, like artificial tears. It may help relieve dryness and scratchiness. Make sure to use eye drops that do not contain redness removers. Lubricating gels can be used before bed to prevent the cornea (the front of the eye) from drying out because your eyelids may not close completely when sleeping.
Taping: Talk with your doctor about taping your top and bottom eyelids together to help protect your front of your eye (cornea) from drying when your eyelids do not close completely during sleep.
Elevate your head when laying down: Keeping your head higher than the rest of your body may reduce swelling and may help relieve pressure on your eyes.
Quit smoking: Smoking (and second hand exposure to smoke) is an important risk factor for thyroid eye disease (TED). If you smoke, quit, and avoid second hand smoke.
Steroids: Swelling in your eyes may be improved by treatment with steroids (such as hydrocortisone or prednisone). Your ophthalmologist may recommend either intravenous or oral medication. Make sure you discuss the risks of use of steroids with your doctor before use.
Pharmaceutical treatments: There are intravenous infusion (putting drugs into a vein) treatments that are FDA-approved medications for the treatment of thyroid eye disease. Researchers are studying new ways to treat TED and several other treatments are in clinical trials. If you’re interested in learning more or seeing if a trial might be right for you, talk to your doctor or visit clinicaltrials.org. Learn more about clinical trials.
Selenium supplements: More research is needed around the effectiveness of selenium supplements. Talk to your doctor before starting any supplements.
Prisms: Thyroid eye disease can cause scar tissue to develop in your eye muscles. This can lead them to become tight and pull your eyes out of alignment, causing double vision. If double vision occurs, glasses containing prisms may be prescribed by your doctor. However, prisms do not work for all people with double vision, and your doctor may recommend patching one eye for temporary relief or eye muscle surgery as a more effective option when changes have stabilized.
Eyelid surgery: When you have thyroid eye disease, the eyelids are usually more widely open with a “startled look” because the muscles in the eyelids may tighten and pull the upper lid up and the lower lid down. You may have difficulty closing your eyelids, leaving the front of the eye (cornea) more exposed, which causes tearing, irritation and susceptibility to developing a corneal ulcer. Eyelid surgery may help reduce exposure of the cornea.
Eye Muscle Surgery: Eye muscle surgery may help correct your double vision by moving the affected muscle(s) farther back from its original position on the eyeball. This surgery will help to correct your double vision when reading and looking straight ahead. Sometimes, you may need more than one surgery to get effective results.
Orbital Decompression Surgery: Thyroid eye disease can cause swollen tissues around the eye that compresses the optic nerve. The optic nerve provides the connection between your eye and the brain. When the nerve is compressed, color vision becomes abnormal, lights may seem dimmer than usual, and the sharpness of the vision decreases. Orbital decompression surgery can be done to improve your vision. The surgery makes the eye socket bigger or removes some of the excess tissue. When the nerve is compressed, the goal of surgery is to get the eye and the inflamed tissue more space and decrease pressure on the optic nerve. Even when the optic nerve function is not compromised, orbital decompression may be used to restore comfort and appearance by reducing the bulging of the eyes. If orbital decompression surgery is recommended, it is usually performed prior to eye muscle surgery and/or eyelid surgery, if needed.
Your ophthalmologist will require some time for your thyroid eye disease to stabilize before recommending surgery. Typically, the active or inflammatory stage of TED lasts one to three years. During this time, your ophthalmologist will avoid surgically treating your symptoms unless your vision is threatened. In cases such as a corneal ulcer or optic nerve compression urgent surgery may be recommended.
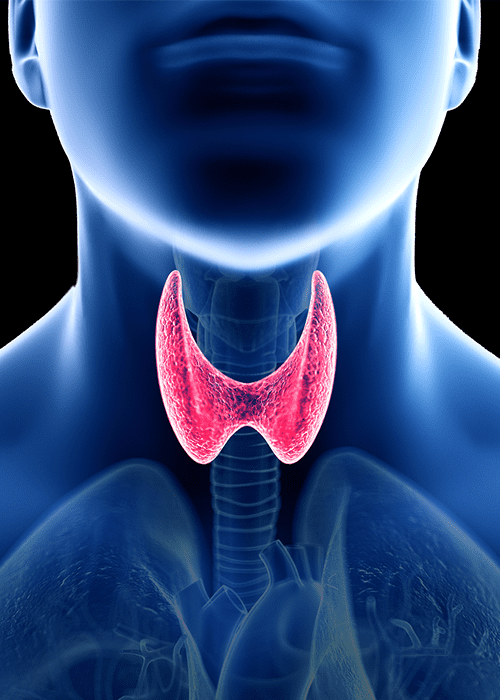
The Thyroid Gland and Important Terms
Thyroid Gland: The thyroid gland is located in the front of your neck. It produces thyroid hormones that are sent to the blood and carried around to other parts of your body. These hormones help your body use energy, stay warm and keep the brain, heart, muscles, and other organs working normally. The thyroid gland can become overactive (hyperthyroidism) or underactive (hypothyroidism). This is most often due to an autoimmune disease in your body.
Hyperthyroidism: Hyperthyroidism is a condition where the thyroid gland is stimulated by the immune system to produce more thyroid hormones than are needed by the body. Symptoms may include weight loss, nervousness, irritability, increased perspiration, fast heart rate, hand tremors, difficulty sleeping, thinning of the skin, brittle hair, and frequent bowel movements.
Hypothyroidism: Hypothyroidism is a condition where thyroid gland function is blocked by the immune system and not enough thyroid hormone is produced for the body’s needs. Symptoms may include feeling cold and tired, having drier skin, becoming forgetful and depressed, and having constipation.
Autoimmune disease: If you have an autoimmune disease, your immune system mistakenly attacks your body. Autoimmune diseases can affect many parts of the body. The cause of autoimmune diseases is largely unknown.
Graves’ Eye Disease: Graves’ Eye Disease is an autoimmune disease which primarily affects the thyroid gland. Other parts of the body may be affected, including eyes and skin. It is the most common cause of hyperthyroidism.
The Thyroid Gland
How does thyroid eye disease affect mental health?
Thyroid eye disease can cause eye pain, double vision, loss of vision, and changes to your appearance which may impact your quality of life. The impacts of TED may lead you to experience to depression, anxiety, loss of independence, and reduced self-confidence. You may have a decreased desire to socialize with others, have trouble with productivity at school or work, and stop doing activities you once enjoyed.
To help support your mental health, consider the following:
- Talk to your doctor: Talk to your doctor about any changes to your emotional well-being. Ask questions on how TED will affect your daily life and work.
- Seek support: Seek out support groups of others who are going through TED. The TED Community Organization and the Graves’ Disease and Thyroid Foundation offers support groups for people with Graves’ disease, Thyroid Eye Disease, and other thyroid conditions. These groups can help you learn about your condition, share your experience, and find support.
- Connect with others: Stay connected with friends and family to keep you from feeling isolated. Consider involving your closest family and friends in your treatment, let them know how they can support you during this process.
- Take time to enjoy life: Take part in activities or hobbies that make you happy.
- Exercise: Exercise can help symptoms of depression or anxiety and make you feel better. Talk to your health care professional to determine what exercise routine may work best for you, especially if you have changes to your vision due to TED.
To learn more, check out the following resources:
National Alliance on Mental Illness (NAMI): Warning signs and symptoms
American Psychological Association: Depression
Centers for Disease Control and Prevention (CDC): The Mental Health of People with Disabilities
Centers for Disease Control and Prevention (CDC): Vision Loss and Mental Health
This resource was made possible by the generous support of:
Regardless of funding source, Prevent Blindness retains full independence over all our health education content, policy positions, advocacy efforts, and programmatic decisions.