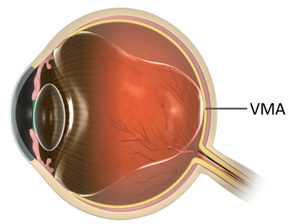
As a person gets older, the central gel that fills the eye called the vitreous liquefies and loses shape, leading to separation of the vitreous from the retina located at the back of the eye. This separation is a normal part of aging and is called a posterior vitreous detachment (PVD). However, if the separation is not complete, small areas of the vitreous can remain attached to the macula, the part of the retina that is responsible for your sharp, central vision. If this attachment causes the retina to be pulled, the condition is called symptomatic vitreomacular adhesion (symptomatic VMA). It can lead to distortion of your vision, a decrease in vision, and/or a loss of central vision in more severe cases.
Symptomatic VMA and Refractive Error
Who is at Risk for Symptomatic VMA?
Much like posterior vitreous detachment (PVD), symptomatic VMA typically occurs in individuals over the age of 50 and is most common in elderly individuals over the age of 70. It is also slightly more common in women and nearsighted individuals.
What are the Signs and Symptoms of Symptomatic VMA?
Symptomatic VMA may lead to various symptoms such as distortion of your vision, a decrease in vision, and/or a loss of central vision.

Distorted Vision
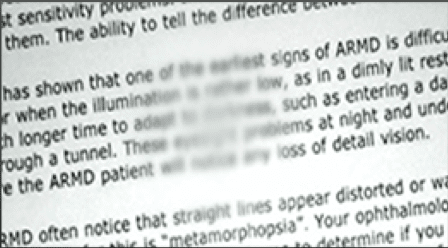
Loss of Central Vision
How Does Symptomatic VMA Damage My Eyes?
Symptomatic VMA is a result of the macula, center of the retina, being pulled. This pulling disrupts the retinal architecture and can lead to several problems such as vitreomacular traction and full thickness macular hole.
How Do Eye Doctors Check for Symptomatic VMA?
Eye care professionals are able to detect symptomatic VMA through a complete, dilated eye examination including an optical coherence tomography (OCT) examination. During the eye exam, the eye doctor widens the pupil of the eye (dilates the eye) with eye drops to allow a closer look at the inside of the eye. The OCT examination provides images of the back of the eye including the vitreous and retina, allowing eye doctors to accurately diagnose symptomatic VMA. Diagnosis is difficult without an OCT examination.
How Do Eye Doctors Treat Symptomatic VMA?
Current options for patients with symptomatic VMA are “watchful waiting,” surgical removal of the vitreous gel (vitrectomy), and intraocular injection of medication.
Watchful Waiting
Many patients undergo a period of “watchful waiting” during which symptoms are not treated until they get severe enough to warrant action.
Surgery
A doctor uses a small, combined cutting-suction instrument to remove part of the vitreous gel of your eye to relieve the adhesion between the retina and vitreous. The doctor then replaces the removed vitreous gel with fluid or a temporary gas bubble. This procedure is called a vitrectomy. Vitrectomy is used as a surgical option when patients have or are at risk of severe visual disturbance and/or loss of central vision.
Medication
Medication that is injected into the eye can be used as a treatment option for symptomatic VMA. It can lead to the release of the adhesion between the vitreous and the macula.